In the trenchesSponges stop troops from bleeding out
Researchers at MIT have created special sponges that can help stop bleeding almost instantaneously; the sponges have been given a coating that includes thrombin, a clotting agent found in blood
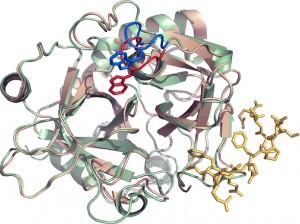
Rendering of the nanoscale coating containing thrombin to aid wound clotting // Source: bostinno.com
Thanks to a new medical breakthrough, soldiers on the battlefield now have a significantly higher chance of surviving injuries on the battlefield.
Researchers at MIT have created special sponges that can help stop bleeding almost instantaneously. The sponges have been given a coating that includes thrombin, a clotting agent found in blood.
Once coated, these sponges can be stored stably and easily carried onto the battlefield by troops.
“The ability to easily package the blood-clotting agent in this sponge system is very appealing because you can pack them, store them, and then pull them out rapidly,” said Paula Hammond, a professor at MIT’S Department of Chemical Engineering and the lead researcher on the project.
In tests, coated sponges were able to stop bleeding in test animals within sixty seconds, while uncoated sponges stopped bleeding in at least 150 seconds. In contrast, a gauze patch applied for twelve minutes did not stop the bleeding.
In addition the sponges themselves are malleable so they can be molded to fit the shape of any wound.
“Now we have an alternative that could be used without applying a large amount of pressure and can conform to a variety of wounds, because the sponges are so malleable,” said Anita Shukla, the lead author of the paper detailing Hammond’s team’s discovery.
According to Hammond the sponges are far superior to existing techniques to stop uncontrollable bleeding, the leading cause of injury-related death in battle. Torniquets are not always applicable to wounds on the neck or other parts of the body, while other clotting techniques like fibrin dressing or zeolite powders are difficult to apply, result in adverse reactions, or have short shelf lives.
Borrowing a technique from civilian hospitals, where a highly absorbent gelatin sponge soaked in thrombin is applied to a wound, Hammond and her team decided to pre-coat sponges to make them suitable downrange.
In civilian hospitals, the sponges must be soaked in liquid thrombin before they are applied to a wound, making them impractical for troops. To create a military version of this technique, Hammond’s team developed a special nanoscale biological coating that could be sprayed onto sponges in layers.
According to David King, a trauma surgeon at Massachusetts General Hospital who has served in Afghanistan as chief of trauma surgery, the coating allows a large amount of thrombin to be crammed into the sponges as even its interior fibers are covered.
“All of the existing hemostatic materials suffer from the same limitation, which is being able to deliver a dense enough package of hemostatic material to the bleeding site. That’s why this new material is exciting,” said King.
Hammond’s team is currently awaiting approval for the sponges by the U.S. Food and Drug Administration. In the meantime, Hammond is working to create a sponge that contains both blood-clotting agents and an antibiotic.
