Researchers develop an Ebola vaccine
Researchers develop an experimental vaccine that cures the Ebola virus by targeting its genetic material; trouble is, the Ebola vaccine can only work if it is administered within thirty minutes, which is an impracticality among civilian populations; the vaccine is a viable possibility within a research facility, so it may be used to protect the researchers themselves
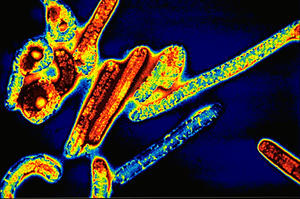
The Ebola virus // Source: britannica.com
One of the world’s deadliest pathogens may finally be contained. After decades of unsuccessful research, a collaboration based out of the U.S. Army’s labs at Fort Detrick, Maryland has devised an experimental vaccine that cures the Ebola virus by targeting its genetic material.
Katie Drummond writes that the injection uses a novel technique, called RNA interference, to stop viral cells from replicating. Scientists packaged RNA snippets into particles that were then injected into four rhesus monkeys, who had been infected with a dose of Ebola which was 30,000 times more potent than the virus’ most lethal strain, which already has a measly 10 percent survival rate. The snippets latched onto key viral proteins, and cured all four monkeys after a week of daily injections.
“Over the past decade, we have evaluated numerous therapeutic approaches for the treatment of lethal viruses, such as Ebola,” the study’s co-author, Dr. Lisa E. Hensley, said. “None of them have conferred complete protection to Ebola virus-infected primates — until now.”
Drummond notes that the study of dangerous pathogens, like Ebola, is tricky. Because cures for the exotic viruses are so rare, researchers are anxious to make progress. This same dearth of treatment options, however, means that even a carefully monitored lab experiment can pose a fatal threat.
This is why the U.S. Army has a vested interest in curbing the potentially lethal exposures of researchers and scientists to deadly pathogens. Last year, a German scientist was quarantined for eight days after accidentally sticking herself with an Ebola infected needle, and similar incidents have occurred in the United States and Russia. The risks are not limited to Ebola: last year, the USAMRIID (United States Army Medical Research Institute of Infectious Diseases) labs — the same facilities doing this study — were temporarily shut down because of problems keeping tabs on microbes and biomaterials. Last summer, a University of Chicago microbiologist died — and an autopsy revealed he had plague bacteria in his blood. The researcher was working with a weakened vaccine strain of Yersinia pestis, intended for the development of vaccines against plague (see “Mystery surrounds University of Chicago ‘plague death’ victim,” 24 September 2009 HSNW).
Exposures caused by lab mishaps may be the most feasible targets for the new method. Right now, the Ebola vaccine can only work if it is administered within thirty minutes — an impracticality among civilian populations, but a viable possibility within a research facility.
“To wait for the next incident to happen in a high-containment laboratory before any progress takes place seems intolerable,” Heinz Feldmann, a virologist with the National Institute of Allergy and Infectious Diseases, writes in a commentary accompanying the study. “We also urgently need to improve outbreak support and go beyond transmission control, and actually provide specific care for affected individuals, which should be an ethical obligation for all of us.”
For now, scientists are focused on demonstrating the proof-of-concept study in more animal trials, before even moving onto human subjects. The method, if successful, could also have widespread applications in treating other viral agents.
