-
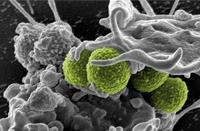
Antibiotic “smart bomb” targets specific strains of bacteria
Researchers have developed a de facto antibiotic “smart bomb” that can identify specific strains of bacteria and sever their DNA, eliminating the infection. The technique offers a potential approach to treat infections by multi-drug resistant bacteria.
-
-
Faster way to spot bacteria-tainted food -- and prevent illness
The regular appearance of food poisoning in the news, including a recent event that led to the recall of more than 33,000 pounds of chicken, drives home the need for better bacterial detection long before meats and produce make it to the dinner table.
-
-
FDA allows use of antibiotics in livestock despite “high risk” to humans

The Center for Disease Control and Prevention (CDC) has recently confirmed the link between antibiotic use on industrial farms and the rise of antibiotic resistance, saying there is “strong scientific evidence of a link between antibiotic use in food animals and antibiotic resistance in humans,” and warns of “potentially catastrophic consequences” if resistance is not slowed. The Food and Drug Administration (FDA), however, has quietly allowed thirty potentially harmful antibiotics, including eighteen rated as “high risk,” to remain on the market as additives in farm animal feed and water. The FDA first recognized the risks from the use of antibiotics in animal feed in 1977, when it proposed to withdraw approvals for animal feed containing penicillin and most tetracyclines. The agency has not followed through on its own findings – and has fought court orders to do so — and today 70 percent of all medically important antibiotics sold in the United States are sold for use in livestock production — not on humans.
-
-
New anthrax-killing virus could offer new ways to detect, treat, and decontaminate anthrax bacillus
From a zebra carcass on the plains of Namibia in Southern Africa, researchers have discovered a new, unusually large virus (or bacteriophage) which infects the bacterium that causes anthrax. The novel bacteriophage could eventually open up new ways to detect, treat, or decontaminate the anthrax bacillus and its relatives that cause food poisoning. Bacteriophages are often highly specific to a particular strain of bacteria, and when they were first discovered in the early twentieth century there was strong interest in them as antimicrobial agents. The discovery of penicillin and other antibiotics, however, eclipsed phage treatments in the West, although research continued in the Soviet Union.
-
-
Drug alternatives to antibiotics come with their own problems
Researchers have been probing the long-term effectiveness of drugs currently being developed by the pharmaceutical industry. These drugs are intended for use in place of antibiotics, and they work by limiting the symptoms caused by a bug or virus in the body, rather than killing it outright. These treatments are designed to avoid the problem of infections becoming resistant to treatment, which has become widespread with antibiotics, but scientists caution that people given damage limitation treatments may appear healthy, but carry high levels of infection and so may be more likely to pass on disease. In addition, people with lesser symptoms could remain undiagnosed and add to the spread of disease.
-
-
Engineering student develops early detection methods for E. coli bacteria
Currently, it can take several days to detect bacteria in meat. A biomedical engineering graduate student at the University of New Mexico is working on ways quickly to detect Escherichia coli or E. coli bacteria in meat before it reaches the consumer. “If we are able to detect E. coli very early on in the beef chain, for example, in cows that are in the pasture or in beef samples from the slaughterhouse, we can prevent further contamination down the line, thereby mitigating the effect of mass recalls and illness,” she says.
-
-
Substitute for conventional antibiotics: Researchers discover a protein that kills bacteria
Bacterial resistance is a natural process. Over the past sixty years or so, however, the misuse and overuse of antibiotics has pushed more and more bacteria to become more and more resistant, undermining one of the pillars of modern health care. Bacterial resistance to antibiotics has developed faster than the production of new antibiotics, making bacterial infections increasingly difficult to treat. Scientists worry that a particularly virulent and deadly “superbug” could one day join the ranks of existing untreatable bacteria, causing a public health catastrophe comparable with the Black Death. Now, researchers have discovered a protein that kills bacteria. The isolation of this protein, produced by a virus that attacks bacteria, is a major step toward developing a substitute for conventional antibiotics.
-
-
California lawmakers propose restricting use of antibiotics in livestock

The growth of antibiotic-resistant bacteria in humans has been attributed to the increasing use of antibiotics in livestock. The Centers for Disease Control and Prevention(CDC) estimates that antibiotic-resistant bacteria infect more than two million Americans a year,killing at least 23,000 of them. California legislators are proposing new laws to restrict the use of antibiotics in livestock.
-
-
Economists propose market-driven solutions to the problem of antibiotic use in agriculture
Fifty-one tons of antibiotics are consumed daily in the United States, of which 80 percent are used in agriculture. To minimize the overuse of antibiotics in livestock, Aidan Hollis of the University of Calgary is proposing the imposition of an antibiotic tax on food producers, thus encouraging them to distinguish between good and bad use of antibiotics, since the fee would force farmers to purchase antibiotics only when needed to treat sick animals and not for non-illness purposes.Timothy Richards of Arizona State University says that more regulations or a tax would run the risk of harming the agriculture industry. He says that farmers and ranchers should clearly label their products as containing or not containing antibiotics, and then market dynamics would operate by “letting people follow labels and buy or not buy meats where antibiotics are used.”
-
-
Superbugs were found breeding, spreading in sewage plants
Antibiotic-resistant bacteria have been raising alarms for years, particularly in hospital environments where public health officials fear they can be transferred from patient to patient and are very difficult to treat. Bacteria harboring the encoding gene that makes them resistant have been found on every continent except for Antarctica. Tests at two wastewater treatment plants in northern China revealed antibiotic-resistant bacteria —“superbugs” carrying New Delhi Metallo-beta-lactamase (NDM-1), a multidrug-resistant gene first identified in India in 2010 — were not only escaping purification but also breeding and spreading their dangerous cargo. NDM-1 is able to make such common bacteria as E. coli, salmonella, and K. pneumonias resistant to even the strongest available antibiotics.
-
-
New test for detecting newly emerging strains of drug-resistant superbug
Molecular assays for MRSA are used in active surveillance programs to identify colonized patients rapidly. Active surveillance is a proven strategy to reduce transmission in healthcare settings and it helps prevent infection in vulnerable patients. BD Diagnostics has received FDA clearance to market the BD MAX MRSA XT Assay for use on the BD MAX System. This is the second assay from BD Diagnostics capable of detecting newly emerging MRSA strains with the novel mecC gene.
-
-
Patients infected with drug-resistant bacteria at suburban Chicago hospital
Health authorities in Illinois have placed a suburban Chicago hospital under tight scrutiny after an extremely rare strain of a dangerous drug-resistant strand of flu was found to be connected to a series of operations performed at the hospital. The Centers for Disease Control and Prevention (CDC) has discovered forty-four cases of Illinois patients infected with a particular bacteria, and thirty-eight of those individuals had all recently undergone an endoscopic procedure at Advocate Lutheran General Hospital, located in Park Ridge west of Chicago, in the past year.
-
-
Extensive use of antibiotics in agriculture creating public health crisis

In the United States, 80 percent of the antibiotics are consumed in agriculture and aquaculture for the purpose of increasing food production. This flood of antibiotics released into the environment — sprayed on fruit trees and fed to the likes of livestock, poultry, and salmon, among other uses — has led bacteria to evolve.Mounting evidence shows resistant pathogens are emerging in the wake of this veritable flood of antibiotics — resulting in an increase in bacteria that is immune to available treatments. Scientists say that if the problem is left unchecked, this will create a health crisis on a global scale.
-
-
Superbugs discovered to be breeding in sewage plants
Rice University study finds that two wastewater treatment plants in China fail to kill antibiotic-resistant bacteria. The bacteria were not only escaping purification but also breeding and spreading their dangerous cargo.
-
-
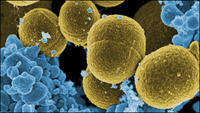
New weapon in the war on superbugs
In the arms race between bacteria and modern medicine, bacteria have gained an edge. In recent decades, bacterial resistance to antibiotics has developed faster than the production of new antibiotics, making bacterial infections increasingly difficult to treat. Scientists worry that a particularly virulent and deadly “superbug” could one day join the ranks of existing untreatable bacteria, causing a public health catastrophe comparable with the Black Death.
-
- All
- Regional
- Water
- Biometrics
- Borders/Immig
- Business
- Cybersecurity
- Detection
- Disasters
- Government
- Infrastructure
- International
- Public health
- Public Safety
- Communication interoperabillity
- Emergency services
- Emergency medical services
- Fire
- First response
- IEDs
- Law Enforcement
- Law Enforcement Technology
- Military technology
- Nonlethal weapons
- Nuclear weapons
- Personal protection equipment
- Police
- Notification /alert systems
- Situational awareness
- Weapons systems
- Sci-Tech
- Sector Reports
- Surveillance
- Transportation
Advertising & Marketing: advertise@newswirepubs.com
Editorial: editor@newswirepubs.com
General: info@newswirepubs.com
2010-2011 © News Wire Publications, LLC News Wire Publications, LLC
220 Old Country Road | Suite 200 | Mineola | New York | 11501
Permissions and Policies
Editorial: editor@newswirepubs.com
General: info@newswirepubs.com
2010-2011 © News Wire Publications, LLC News Wire Publications, LLC
220 Old Country Road | Suite 200 | Mineola | New York | 11501
Permissions and Policies
